Introduction
The COVID-19 pandemic exposed deep-seated inequalities across the United States, disproportionately impacting marginalized communities. New Mexico, a southwestern state in the USA, presents a unique demographic profile with a significant minority population and high poverty rates, potentially amplifying its vulnerability to the pandemic’s negative social consequences. To effectively address these challenges, understanding community-level vulnerability is crucial, especially when resources need to be allocated efficiently across different time zones in New Mexico and the USA.
Following the initial COVID-19 case in New Mexico on March 11, 2020, we developed a county-level vulnerability index to pinpoint communities at heightened risk. This index utilizes a generalized propensity score model, incorporating key sociodemographic factors to predict county-level viral exposure and the subsequent risk of adverse social outcomes such as job losses and mental health issues. We considered four essential static sociodemographic variables relevant to New Mexico: population size, poverty levels, average household size, and minority population percentage. By iteratively applying our model weekly and normalizing the exposure score, we created a dynamic, time-varying vulnerability index.
Our findings revealed that the relative vulnerability among New Mexico counties fluctuated during the first two months after the pandemic’s onset before stabilizing. Notably, average household size emerged as a significant factor influencing these time-sensitive vulnerability shifts. This adaptable vulnerability index can serve as a valuable decision-making tool for health officials, enabling them to strategically allocate state resources at the county level, ensuring timely and effective interventions across New Mexico, regardless of the specific USA time zone. This framework for creating a location-specific, time-sensitive vulnerability index during a disaster can be applied to other regions and crises, providing a rapid and deployable metric for informed health policy decisions.
1. Background: COVID-19 and Community Vulnerability in New Mexico
The World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020 [1], [2], marking a global health crisis with far-reaching consequences. In the United States, the initial instance of potential community transmission was documented on February 26, 2020 (CDC, 2020). By December 31, 2020, the nation had recorded over 20 million cases and 346,000 deaths [3]. The pandemic’s impact has been uneven, disproportionately affecting racial and ethnic minorities and underserved populations [4], [5], [6], highlighting existing systemic inequalities in the social burdens stemming from such widespread health emergencies. While a certain level of COVID-19 incidence in a less vulnerable community might have limited social repercussions, a similar infection rate in a more vulnerable community can trigger a cascade of negative effects, including unemployment, increased poverty, and mental health crises. This disparity underscores the urgent need to identify and support the most vulnerable communities, particularly in states with diverse cultural landscapes like New Mexico.
New Mexico, with a population of approximately 2.1 million, possesses a unique demographic composition within the USA. It has the highest percentage of Hispanic or Latino residents (49%) compared to the national average of 19% [7], [8], [9], [10]. Furthermore, New Mexico ranks second in the USA for its percentage of Native American or Alaska Native population (11% versus the 1% national average) [7], [9]. A significant portion of New Mexico’s Native American population, the Diné, resides in the Navajo Nation, the largest Native American reservation by area and second largest by population, located in the state’s northwest region [7]. In total, New Mexico is home to 23 Native American tribes, including 19 Pueblos, predominantly situated in the northern part of the state [11]. Economically, New Mexico faces challenges, ranking among the poorest states in the USA, with around 19% of its population living below the poverty line [12].
These factors—high poverty rates and a large minority population—contribute to the US Centers for Disease Control and Prevention (CDC) classifying New Mexico counties as highly vulnerable to disaster outcomes, including pandemics [13]. The CDC’s Social Vulnerability Index (SVI) assesses this vulnerability using socioeconomic status, household composition, race/ethnicity/language, and housing/transportation themes to determine relative vulnerability across all US counties. In New Mexico, communities with pre-existing vulnerabilities are likely to experience more severe negative consequences from COVID-19, straining both public health systems and the economy. The disproportionate health impact is already evident: as of September 14, 2020, Native American, Alaska Native, and Hispanic/Latino individuals constituted 76% of COVID-19 cases in New Mexico, despite representing only 60% of the state’s population. In contrast, White individuals, who make up 37% of the population, accounted for just 14% of cases [10], [[14]](#b0070].
While the SVI provides a static, nationwide comparison of county vulnerability, it does not adapt to the evolving nature of an ongoing disaster like the COVID-19 pandemic. A time-varying vulnerability index, incorporating real-time COVID-19 burden measurements, can offer a more precise and up-to-date assessment of relative vulnerability to pandemic-related social consequences. Increased case burden can create a feedback loop within a community: rising cases lead to negative outcomes, which, in turn, further escalate case burden. For example, a COVID-19 outbreak at a local business might force closure, causing job losses and financial instability, preventing residents from affording protective measures and increasing infection risk. Furthermore, considering New Mexico’s unique demographic makeup, incorporating sociodemographic variables that reflect disparities within the state’s communities can provide a more nuanced vulnerability measure compared to national-level indices like the SVI.
Our objective was to develop a county-level vulnerability index for New Mexico to identify communities at the highest risk of negative social outcomes as the COVID-19 pandemic progressed. We compiled county-level sociodemographic data representing vulnerabilities specific to New Mexico. Then, we employed a generalized propensity score model to create a generic causal effect measure of COVID-19 case burden in each community. By normalizing this measure, we generated a vulnerability index reflecting the relative county-level vulnerability to negative social outcomes from COVID-19. To initially evaluate our index’s performance, we compared vulnerability rankings with county-level cumulative death and case fatality ratio data. This vulnerability index can serve as a decision support tool for New Mexico state health officials, enabling them to identify community vulnerabilities and allocate resources effectively at the county level. More broadly, this framework can be applied to other locations and contexts to identify at-risk communities during ongoing disasters, providing a valuable tool adaptable across different USA time zones and regions.
2. Methods
2.1. Selection of Sociodemographic Covariates
We identified four key sociodemographic themes that could increase community vulnerability to negative COVID-19 outcomes in New Mexico. First, total population within each county is a critical factor. Population size directly influences infectious disease transmission through community spread [15], [16]. We used total population, rather than population density, because county-level density measures in New Mexico are skewed by urban centers. While New Mexico has four cities with populations exceeding 50,000 (Albuquerque, Las Cruces, Rio Rancho, and Santa Fe) [[10]](#b0050] concentrated in Bernalillo, Doña Ana, Sandoval, and Santa Fe Counties, respectively, much of the state is rural or uninhabited [17]. Although densely populated areas can experience higher cumulative case counts, they often have greater access to social support and healthcare resources compared to rural communities [[15]](#b0075]. Therefore, smaller, rural populations might be at higher risk for negative social outcomes from COVID-19.
Second, the percentage of the population living in poverty is a significant vulnerability factor. New Mexico ranks as the second poorest state in the USA by poverty rate and has the fourth-lowest median household income [12]. Within the state, 20 counties (30%) report at least 20% of residents living below the state-adjusted poverty line [18]. Individuals in poverty may lack access to essential disease prevention resources like masks, clean water, and disinfectants, increasing their infection risk. Lower-income areas may also exhibit lower adherence to stay-at-home orders, potentially accelerating community transmission [19]. COVID-19 infection can financially overwhelm people in poverty, leading to housing insecurity and food scarcity. Lower-income jobs often require on-site presence (e.g., transportation, retail) [[20]](#b0100], increasing vulnerability to job loss due to outbreaks or unpaid sick leave, causing financial strain and potential eviction.
Third, average household size is another crucial covariate. The average US household size is 2.63 people, and New Mexico’s statewide average is similar at 2.64 [10]. However, multigenerational households are common in certain New Mexican cultures, resulting in larger household sizes, ranging from 2.02 to 3.62 across counties [[7]](#b0035]. Areas with larger Hispanic or Latino and Native American populations, like New Mexico, tend to have higher rates of multigenerational households [[21]](#b0105] due to cultural norms, socioeconomic factors, immigration patterns, and health status [22], [23], [24], [25], [[26]](#b0130]. Higher housing density likely contributes to increased virus transmission, as secondary cases per primary case rise, potentially exacerbating negative social outcomes if multiple family members become ill simultaneously.
Fourth, percentage of minority population, defined as those not identifying as “White alone, not Hispanic or Latino” in the US Census, represents a significant vulnerability. New Mexico has a 63% non-White population, compared to the 40% US average [8], [[10]](#b0050], with Native Americans/Alaska Natives at 11% and Hispanic/Latinos at 49% [[7]](#b0035]. Minority populations have been disproportionately affected by COVID-19 [[5]](#b0025], due to biomedical and health inequity factors [[5]](#b0025]. Minority groups often experience higher rates of underlying conditions like heart disease and diabetes, or substance use disorders, increasing their risk of COVID-19 complications and compounding negative social outcomes [4], [5], [6], [[27]](#b0135]. Minority-owned small businesses may also suffer disproportionately from worker illness or closures due to public health mandates.
2.2. Data Sources: COVID-19 and Sociodemographic Covariates
We utilized a generalized propensity score model to predict county-level COVID-19 case exposure (n=33) in New Mexico, using cumulative case counts as an exposure metric (Figure S1). Daily, county-level COVID-19 case data were collected from the New York Times (NYT) from March 11, 2020, to August 3, 2020 [[3]](#b0015]. Following Marvel et al. [[28]](#b0140], we compared our vulnerability index to cumulative COVID-19 deaths from the NYT and the case fatality ratio (calculated as the daily ratio of cumulative cases to deaths, unlagged) over the same period as a preliminary evaluation. We examined lags of one to four weeks between the vulnerability index and COVID-19 outcomes, starting this analysis on April 1, 2020, when at least three New Mexico counties had reported deaths.
County-level total population and sociodemographic variables were obtained from the US Census 2014–2018 American Community Survey (ACS) 5-Year Estimates [[18]](#b0090] (except for Rio Arriba County, from the 2013–2017 ACS 5-Year Estimates) [[18]](#b0090]: percentage of population below the state-adjusted poverty line, average household size, and percentage of non-White population. Aggregated data from recent years were used to capture data for smaller counties in New Mexico. The percentage of non-White population was calculated by subtracting the percentage of “White alone, not Hispanic or Latino” population from 100%. To normalize population distribution, we used the natural log of population to reduce skewness.
2.3. Propensity Score Model Application
We employed a propensity score model to quantitatively assess relative county vulnerability to negative social outcomes from COVID-19. Propensity scores are commonly used in epidemiology to estimate the probability of exposure or treatment in non-randomized studies (see Supporting Information). Our propensity score analysis aimed to create a generic causal effect measure of COVID-19 case burden to assess the pandemic’s social impact. We used a Poisson linear regression model with a population offset term (glm() in R version 4.0.1; Equation (1)), suitable for count data prediction:
| C=β0+β1lnPop+β2Pov+β3(H)+β4(NW) | (1) |
|---|
Where regression coefficients (β) change weekly with cumulative COVID-19 cases (C). To measure relative vulnerability, we normalized the time-varying vulnerability index to a 0-1 scale.
Starting one week after the first reported travel-related COVID-19 cases in New Mexico on March 11, 2020 [29], we iteratively fit our model weekly for 22 weeks (March 18, 2020 – August 12, 2020). Weekly cumulative case counts were used instead of daily data to reduce noise from rapid fluctuations.
3. Results
3.1. Time-Varying Community Vulnerability Index
The four incorporated covariates highlighted sociodemographic variations among New Mexico counties (Fig. 1). Highest population counties are in north-central New Mexico, with one in the south-central region. These high-population counties generally had low to moderate poverty, non-White population percentages, and average household sizes. Lower population counties tended to have higher poverty levels, larger average household sizes, and greater non-White population percentages. McKinley County, within the Navajo Nation, had the highest poverty rate (Fig. S2). Counties with large non-White populations were primarily rural, including Cibola, Rio Arriba, McKinley, San Juan, San Miguel, and Guadalupe.
Fig. 1.
Sociodemographic covariates for New Mexico counties: (a) total population, (b) percentage below poverty line, (c) average household size, (d) percentage non-White population.
Using cumulative COVID-19 cases, we calculated the propensity score model to predict negative social outcomes. Counties with larger average household sizes showed the greatest vulnerability index magnitude changes over time (Fig. 2). Relative county vulnerability fluctuated in the month after New Mexico’s first COVID-19 case (Fig. 3). After the first week, all covariates were statistically significant (p < 0.05; Fig. 3, Table S2). County-specific vulnerability scores are in Supplemental Information, categorized by health districts (Figs. S3–S7).
Fig. 2.
New Mexico county vulnerability indices: (a) week 1, (b) week 22, (c) maximum vulnerability index range.
Fig. 3.
Time series analysis of county vulnerability index in New Mexico (nine highlighted counties).
Regression coefficient time series analysis showed average household size as the most variable covariate (Fig. 4; Table S1). Population had a relatively stable, slightly decreasing coefficient. Poverty percentage was less influential on vulnerability variability and showed an inverse relationship to non-White population percentage.
Fig. 4.
Time series analysis of sociodemographic covariate regression coefficients (intercept excluded).
Preliminary vulnerability index evaluation compared county-level vulnerability to cumulative deaths and case fatality ratio using Spearman correlation (Fig. S8). Although our goal was not to predict cases or deaths, these were the available early pandemic outcome measures. We analyzed 1–4 week lags between vulnerability index and outcomes, starting April 1, 2020. Mean correlation between vulnerability index and cumulative deaths was 0.64–0.66 across lags. Case fatality ratio correlations were lower (0.34–0.36; Fig. S8). For both outcomes, rho values were similar across lags, and significance increased over time, likely due to more counties reporting deaths. Cumulative case count correlations with deaths (0.74–0.78) and case fatality ratio (0.35) were also calculated. While cumulative cases better predicted deaths, our index, designed for broader social outcomes, still adequately captured early COVID-19 outcomes.
4. Discussion
4.1. Time-Varying Community Vulnerability Index Utility
Our generalized propensity score model effectively predicted county-level COVID-19 case exposure, accounting for sociodemographic confounders. This provides a rapid, simple decision support tool for policymakers to allocate resources at the county level and adapt to changing vulnerabilities, such as deploying mobile testing or vaccine distribution, crucial in a state spanning multiple USA time zones. Propensity scores account for confounding variables without specifying causal relationships, making the index broadly applicable to various outcomes.
Average household size was a key, time-varying vulnerability determinant. Initially, larger household sizes predicted higher case numbers, likely due to within-household transmission before widespread awareness and mitigation measures. One week post-first case, New Mexico schools closed [[30]](#b0150], followed by stay-at-home orders [[31]](#b0155] two weeks later, limiting community exposure. Subsequently, the household size regression coefficient became negative for five weeks, suggesting larger households may have become protective, possibly due to reduced external contacts, especially for vulnerable elderly and children in multigenerational homes. However, around Memorial Day weekend, two months post-first case, household size again became positively correlated with cases. This may reflect increased holiday travel, quarantine fatigue, or business reopenings [32], increasing exposure within larger households.
Population, non-White percentage, and poverty percentage had less time-varying influence, but significant correlations existed between covariates (Fig. S9), especially between household size and non-White percentage (0.55). Household size may have captured multiple community vulnerabilities. Sensitivity testing using only household size showed similar time-varying regression coefficient patterns (Fig. S10), indicating its primary role in vulnerability dynamics. Household size has also been linked to infection rates in other respiratory diseases like influenza [33].
4.2. Comparison with Other COVID-19 Vulnerability Indices
Our time-varying vulnerability index differs from static indices like the CDC SVI [[13]](#b0065], offering a more real-time, specific measure for the COVID-19 pandemic. The Surgo Foundation’s COVID-19 vulnerability index [[34]](#b0170], combining SVI factors with COVID-19 specific risks, identifies McKinley, Guadalupe, and Cibola Counties as most vulnerable. Our index also highlights McKinley, but ranks Bernalillo and Doña Ana higher than Surgo’s index.
The NIEHS COVID-19 Pandemic Vulnerability Index [28], [[35]](#b0175] is also time-varying, incorporating sociodemographic and dynamic covariates like COVID-19 outcomes, mobility, and interventions. For August 12, 2020, our index identified Bernalillo, McKinley, and Doña Ana as most vulnerable, while NIEHS ranked Cibola, McKinley, and Lea highest, with Doña Ana and Bernalillo in the top 10. Differences may arise from our model’s New Mexico-specific covariates, compared to nationwide generalizations in CDC and NIEHS indices. Regional variations in culture, policy, and mitigation efforts can limit nationwide index applicability.
While our index targets general social outcomes in New Mexico, it can be modified for specific outcomes like health impacts [[36]](#b0180]. Pre-existing conditions, age, and other health-related factors could be incorporated to assess health vulnerability more directly. Composite indices combining social and epidemiological factors can also assess community health risks [[39]](#b0195].
4.3. Broader Applications and Disaster Adaptability
Our New Mexico-specific vulnerability index framework can be adapted for other regions by adjusting covariates or expanded to national analyses using general US vulnerability factors, similar to CDC and NIEHS indices. Further model development could involve fully dynamic models incorporating time-varying covariate magnitudes like unemployment, homelessness, or mobility to capture feedback loops and refine vulnerability assessments over time.
The generalized propensity score method is transferable to other COVID-19 applications or disasters, provided a suitable exposure proxy exists. For infectious diseases, case counts can be used, but time-scale considerations are important for stable risk measures due to reporting biases. For natural disasters, outcomes like displacement, injuries, or deaths could be used.
5. Conclusions
We developed a time-varying vulnerability index for New Mexico using generalized propensity scores, identifying dynamic community risk during the COVID-19 pandemic. County vulnerabilities fluctuated for two months post-first case and then stabilized. Average household size was a key time-varying determinant, initially positively, then negatively, correlated with vulnerability. The index showed significant correlation with cumulative deaths and case fatality ratio after more deaths were reported, suggesting its predictive value for COVID-19 outcomes. Unlike static measures, our time-varying approach captures dynamic vulnerability during ongoing disasters. This framework can be adapted for other locations and disasters, providing a valuable tool for time-sensitive resource allocation and informed public health responses across the USA and its various time zones.
CRediT authorship contribution statement
Morgan E. Gorris: Conceptualization, Methodology, Writing – original draft. Courtney D. Shelley: Conceptualization, Methodology, Writing – original draft. Sara Y. Del Valle: Writing – review & editing, Supervision, Project administration. Carrie A. Manore: Writing – review & editing, Supervision, Project administration.
Declaration of Competing Interest
The authors declare no competing interests.
Acknowledgements
We thank Dr. Christopher Novak and Dr. Jee Hwang from New Mexico state departments, the New Mexico Department of Health, Presbyterian Healthcare Services, and Dr. Kirsten McCabe at LANL. We gratefully acknowledge support from the Laboratory Directed Research and Development (LDRD) program and the Center for Nonlinear Studies at Los Alamos National Laboratory. M. E. Gorris was funded by a LDRD Director’s Postdoctoral Fellowship. This work is approved for distribution under LA-UR-20-30424. Findings are those of the authors and do not represent official positions. Los Alamos National Laboratory is managed by Triad National Security, LLC, for the National Nuclear Security Administration of the U.S. Department of Energy under contract 89233218CNA000001.
Footnotes
Appendix A Supplementary data is available online at https://doi.org/10.1016/j.hpopen.2021.100052.
Appendix A. Supplementary material
Supplementary data 1
mmc1.pdf (3.3MB, pdf)
References
Associated Data
Supplementary Materials
Supplementary data 1
mmc1.pdf (3.3MB, pdf)
[1] WHO, Novel Coronavirus(2019-nCoV): situation report, 51, World Health Organization (2020).
[2] C. Cucinotta, M. Vanelli, WHO declares COVID-19 a pandemic, Acta Biomed. 91 (1) (2020) 157–160. https://doi.org/10.23750/abm.v91i1.9397.
[3] The New York Times, Coronavirus in the U.S.: latest map and case count, The New York Times (2020). https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html.
[4] M.L. Richardson, et al., Racial and ethnic disparities in hospitalization and death among patients with COVID-19 in 12 hospitals in Michigan, J. Am. Med. Assoc. Intern. Med. 180 (12) (2020) 1721–1729. https://doi.org/10.1001/jamainternmed.2020.4330.
[5] N. Krieger, The public health relevance of racial and ethnic disparities: COVID-19 as the latest example, Am. J. Public Health. 110 (9) (2020) 1347–1349. https://doi.org/10.2105/AJPH.2020.305764.
[6] N.S. Kim, et al., COVID-19 disparities: poorer health outcomes for minority populations, Public Health Rep. 135 (6) (2020) 670–679. https://doi.org/10.1177/0033354920954518.
[7] United States Census Bureau, QuickFacts New Mexico, United States Census Bureau (2019). https://www.census.gov/quickfacts/fact/table/NM,US/PST045219.
[8] United States Census Bureau, 2019 ACS Demographic and Housing Estimates, United States Census Bureau (2019). https://data.census.gov/cedsci/table?q=new%20mexico%20hispanic%20population&g=0400000US35&tid=ACSDP5Y2019.DP05&hidePreview=true.
[9] United States Census Bureau, 2019 ACS Demographic and Housing Estimates United States, United States Census Bureau (2019). https://data.census.gov/cedsci/table?g=0100000US.0400000&y=2019&tid=ACSDP5Y2019.DP05&moe=false&hidePreview=true.
[10] United States Census Bureau, State & County QuickFacts, United States Census Bureau (2019). https://www.census.gov/quickfacts/fact/table/US,NM/PST045219.
[11] Indian Affairs Committee, New Mexico Indian Affairs Department, Indian Affairs Committee (2020). https://www.iad.state.nm.us/demographics.
[12] United States Census Bureau, Poverty in New Mexico, United States Census Bureau (2019). https://www.census.gov/data/tables/2019/demo/saipe/2019-state-and-county.html.
[13] Centers for Disease Control and Prevention, ATSDR’s Social Vulnerability Index (SVI), Centers for Disease Control and Prevention (2018). https://www.atsdr.cdc.gov/placeandhealth/svi/index.html.
[14] New Mexico Department of Health, Coronavirus update, New Mexico Department of Health (2020). https://cv.nmhealth.org/2020/09/coronavirus-update-september-14-2020/.
[15] J. Miller, Urban density and infectious disease, J. Policy Anal. Manage. 7 (4) (1988) 723–727.
[16] R. Lu, et al., Association between urban population density and COVID-19 infection in the 50 US states, medRxiv (2020).
[17] United States Department of Agriculture, New Mexico: 2017 Census of Agriculture, United States Department of Agriculture (2019). https://www.nass.usda.gov/Publications/AgCensus/2017/Online_Resources/County_Profiles/New_Mexico/cp99035.pdf.
[18] United States Census Bureau, 2014-2018 ACS 5-Year Estimates, United States Census Bureau (2018). https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t.
[19] M.R. Slavinski, et al., Association of income inequality with adherence to stay-at-home orders and COVID-19 infection rates in the United States, J. Am. Med. Assoc. Netw. Open. 3 (10) (2020) e2023698. https://doi.org/10.1001/jamanetworkopen.2020.23698.
[20] S.I. Rogers, Essential workers and COVID-19: understanding income and demographic disparities, SSRN (2020).
[21] Pew Research Center, A rising share of young adults live in multigenerational households, Pew Research Center (2018). https://www.pewresearch.org/social-trends/2018/10/18/a-rising-share-of-young-adults-live-in-multigenerational-households/.
[22] R.A. Black, S. Timberlake, Multigenerational households and health in later life: exploring variations by race and ethnicity, J. Gerontol. Ser. B. 69 (1) (2014) 149–159. https://doi.org/10.1093/geronb/gbt007.
[23] Z. Tian, V.A. Freedman, D.A. Schoeni, Living arrangements of older adults in China: variations by socioeconomic status, J. Gerontol. Ser. B. 74 (4) (2019) 651–661. https://doi.org/10.1093/geronb/gby040.
[24] J.S. Wilmoth, Multigenerational coresidence in the United States: 1940-2000, J. Gerontol. Ser. B. 67 (2) (2012) 252–263. https://doi.org/10.1093/geronb/gbr122.
[25] K.M. Werner, et al., Racial and ethnic differences in multigenerational living: exploring economic need and cultural norms, J. Marriage Fam. 77 (4) (2015) 958–975. https://doi.org/10.1111/jomf.12197.
[26] R.S. Brown, et al., Multigenerational households in the United States, Population Reference Bureau (2017).
[27] Centers for Disease Control and Prevention, Health equity considerations and racial and ethnic minority groups, Centers for Disease Control and Prevention (2020). https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-minorities.html.
[28] S. Marvel, et al., Development of a COVID-19 pandemic vulnerability index, medRxiv (2020).
[29] New Mexico Department of Health, NM confirms first cases of COVID-19, New Mexico Department of Health (2020). https://cv.nmhealth.org/2020/03/nm-confirms-first-cases-of-covid-19/.
[30] K. Porter, New Mexico public schools to close for three weeks, Albuquerque Journal (2020).
[31] Office of Governor Michelle Lujan Grisham, Public health emergency order, Office of Governor Michelle Lujan Grisham (2020).
[32] P. Monk, New Mexico enters phase one of reopening, KOB4 (2020).
[33] J.T. McCrone, et al., Household structure and influenza risk, Epidemiology. 29 (6) (2018) 844–853. https://doi.org/10.1097/EDE.0000000000000892.
[34] The Surgo Foundation, COVID-19 vulnerability index, The Surgo Foundation (2020). https://surgofoundation.org/covid-19-vulnerability-index/.
[35] National Institute of Environmental Health Sciences, NIH COVID-19 vulnerability index, National Institute of Environmental Health Sciences (2020). https://covid19.niehs.nih.gov/.
[36] A.K. Hamadani, et al., Household and community-level factors associated with SARS-CoV-2 infection in Bangladesh, medRxiv (2020).
[37] C. Stokes, et al., Spatiotemporal analysis of COVID-19 확진자 패턴과 사회경제적 요인과의 관계 분석, medRxiv (2020).
[38] Centers for Disease Control and Prevention, Older adults at increased risk of severe illness, Centers for Disease Control and Prevention (2020). https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html.
[39] M.J. Pantaleo, et al., Development of a composite social vulnerability and health index for hurricane emergencies, Disaster Med. Public Health Prep. 10 (1) (2016) 112–118. https://doi.org/10.1017/dmp.2015.48.
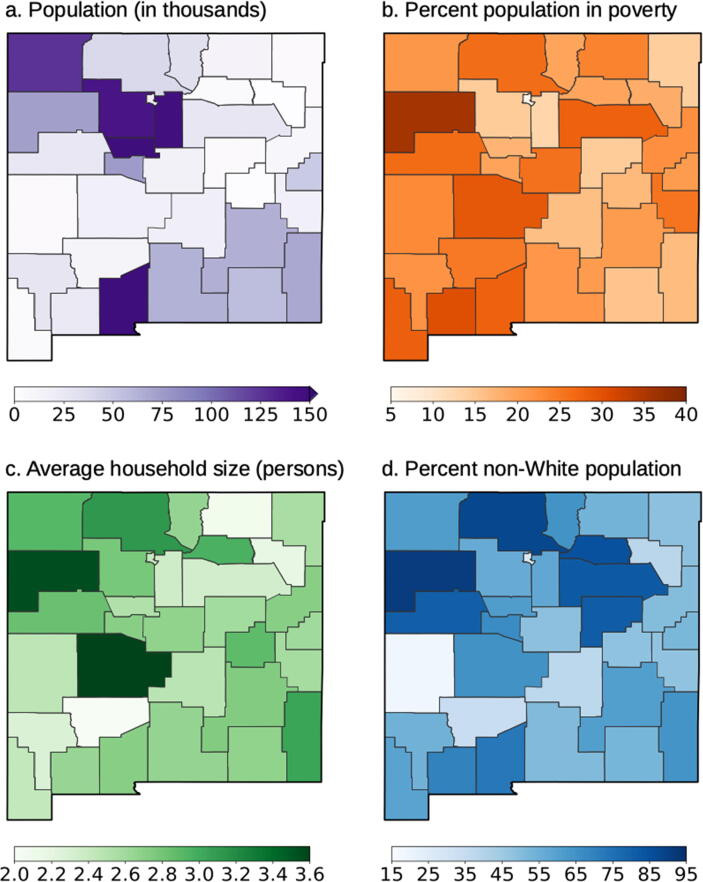
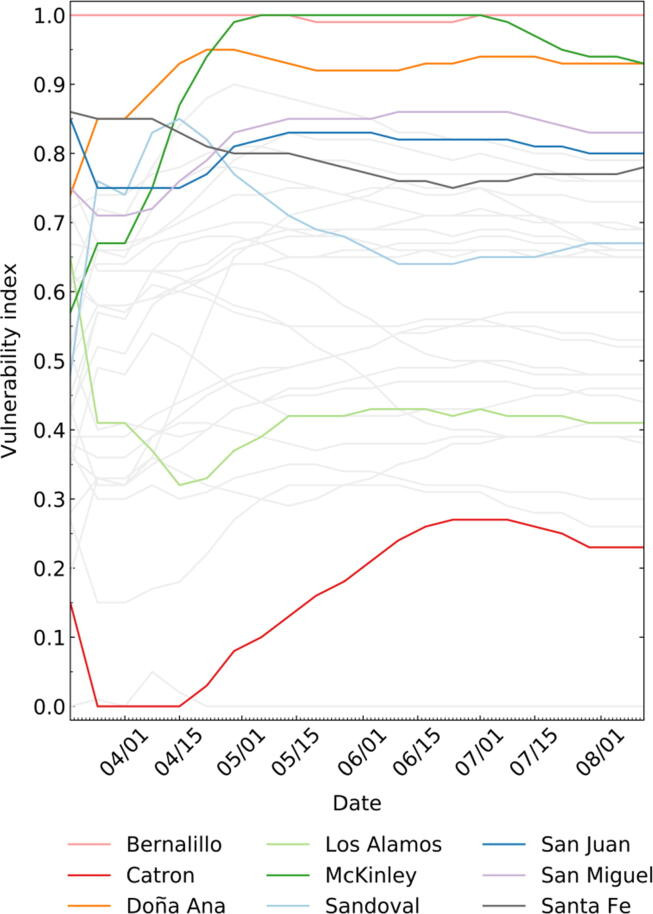 Fig. 3
Fig. 3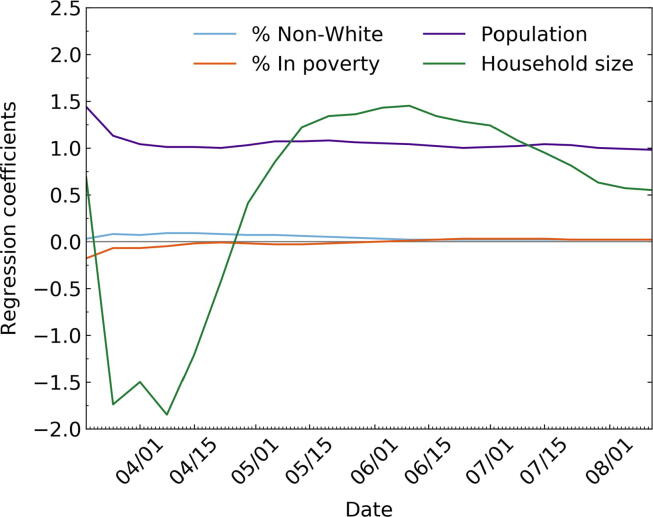 Fig. 4
Fig. 4